Cholesterol was first isolated from gallstones in 1784. Since then 13 researchers have won the Nobel Prize for work centred primarily on cholesterol.
But this article is about much more than cholesterol in all its various forms. There is lots of information so let’s begin with The Take-away. In the last article you learned about why you have to get your Homocysteine levels measured. In this one you’ll find out why you also need to get your LDL, VLDL and HDL-Cholesterols measured along with your Triglycerides.
Cholesterol is not all bad news. Cholesterol is one of the fats in your blood. Your body uses it to make cell membranes, vitamin D and hormones. Specifically in the case of the very important secosteroid hormone, the so-called “Vitamin” D, sunlight acting on the 7-dehydrocholesterol in your skin converts it to cholecalciferol – Vitamin D3. And Vitamin D is critical to so many aspects of your health that it will be covered in later articles.
Triglycerides while not a type of cholesterol, are types of fat found in the blood and are associated with excess weight, excess alcohol consumption and diabetes. Triglycerides should always be measured at the same time as cholesterols and homocysteine.
In the 1950s and 1960s the race was on for a number of companies, each of which wanted to hit the mother lode, and create better health by finding some drug that would block at least one of the steps in the synthesis of cholesterol from acetyl-coenzyme A (CoA) in the body. The first commercially available drug, Triparanol, introduced in 1959 was withdrawn in the early 1960s because it caused cataracts.1 Anytime a foreign substance is introduced into the body side effects are almost inevitable. This would be a challenge for all cholesterol -lowering drugs.
By the 1980s and early 1990s the research on cholesterol was interpreted by the medical community as saying that ALL cholesterol is bad. That is ALL types of cholesterol were viewed as a causative factor for cardiovascular Disease (CVD). So the great goal of most doctors and of the medical establishment in the 1970s and 80’s was to lower ALL cholesterol. This was true even though John Gofman in 1949 at UC Berkeley, found not only that heart attacks correlated with elevated levels of blood cholesterol but also that the cholesterol correlated with heart attacks was contained in low density lipoprotein (LDL)2 He also observed that heart attacks were less frequent when the blood contained elevated levels of high density lipoprotein (HDL).3
Technically LDL and HDL are not cholesterol, but proteins that transport cholesterol to our cells. Cholesterol is neither water soluble nor blood soluble so it needs to be transported by a protein. So when we talk about cholesterol levels we are actually measuring the lipoproteins combined with cholesterol that transport cholesterol. Thus the research on cholesterol is really about which lipoproteins carrying cholesterol are good and which are bad; and what ratio should we have of the different lipoproteins for optimum cardio-vascular health.
Triglycerides
Triglycerides while not a type of cholesterol, are 3 types of fat found in the blood and are associated with excess weight, excess alcohol consumption, diabetes and CVD. Our lipoproteins also carry these three fats that make up what we call triglycerides: mono-unsaturated, saturated and poly-unsaturated. Triglycerides (TG) should always be measured at the same time as your lipoproteins (cholesterols) and homocysteine. They are an independent risk factor for CVD and their role in promoting CVD was first suggested by JR Moreton in the prestigious journal Science in 1947.4
AFH Stalenhoef and J de Graaf noted in 2008 that studies showed “fasting triglycerides increase the adjusted hazard ratios for cardiovascular disease risk 1.7× (comparing upper with lower tertile), and nonfasting levels around 2.0×.”5 In other words knowing and controlling your triglyceride levels is important.
A 2009 meta review by WB Kannel and RS Vasan noted that the “failure to catabolize triglyceride-rich lipoproteins (TRL) efficiently appears to be linked to accelerated atherogenesis since TRL appear to be proinflammatory, cause endothelial dysfunction , upregulate expression of endothelial adhesion molecules and promote macrophage chemotaxis. TRL are especially prone to enter the arterial wall where they are ingested by macrophages (analogous to oxidized LDL), to then become foam cells. Retention of these TRL in the vascular wall also traps the more atherogenic small LDL-Cholesterol particles”.6
While they don’t see triglycerides (TG) as an independent risk factor they do conclude that it is an important co-factor: ”High TG merits consideration as a prominent CVD risk factor because this often identifies candidates for CVD with insulin resistance, highly atherogenic small LDL remnant particles, lower values of HDL-Cholesterol, and other manifestations of the metabolic syndrome. The CVD risk of elevated LDL-Cholesterol is enhanced by coexistent hypertriglyceridemia and lowering both lipid fractions appears superior to reducing LDL-Cholesterol alone. Recent epidemiological studies have underscored the associations of both fasting and non-fasting TG with CVD risk.”6 They also note that the level of triglycerides is increasing in the population. Mean levels in adults (20-74 years) ”have increased from 114 mg/dl in 1976–1980 to 122 mg/dl in 1999–2002” and “to 129.5 mg/dl in 2003–4” while approximately “13% of the US population (27 million people) have TG exceeding 200 mg/dl”.6
Very Low Density Lipoprotein (VLDL) contains the highest levels of triglyceride. High levels of VLDL are linked to the risk of CVD, while large VLDL particles are associated with hypertension – high blood pressure. VLDL is typically estimated as a percentage of triglyceride. 5 to 30 mg/dL is considered a normal range.7
By the 1990s the research literature and the medical establishment was catching up with Gofman and were beginning to suggest that low-density lipoprotein (LDL) was the culprit, while HDL was good.
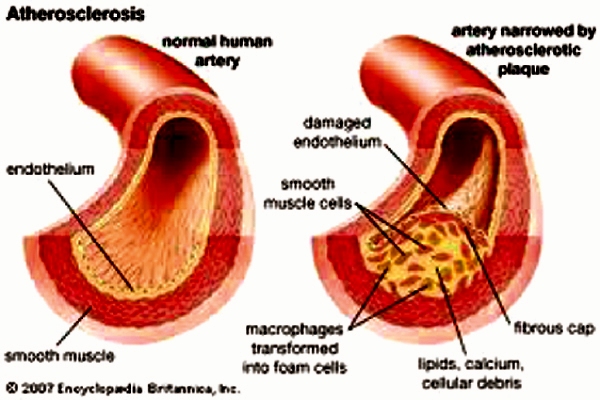
By 1997 it was found that the so-called bad “cholesterol”, LDL, is only bad once it is oxidized. An extensive review article concluded that antioxidants may very well reduce the risk of
atherosclerosis by helping produce LDL that is resistant to oxidative modification. This in
turn reduces the initial phases of “hardening of the arteries”, namely the fatty streak.
Antioxidants also stabilize the arterial plaque where it is most likely to rupture (in the
oxidized LDL laden foam cell layer of the plaque) and cause a heart attack. It may also
reduce the size of the plaque thus reducing constriction or “narrowing” of the artery.8
The same year it was reported that a high dose of antioxidants (800 IU of Vitamin E, 1000 mg of Vitamin C and 24mg of beta-carotene – provitamin A) reduced the susceptibility of LDL to oxidation in patients with cardiovascular disease.9
This finding was reinforced by the results of a study reported in 2005. This study examined the relationship between oxidized LDL (oxLDL) and CVD/CHD. This study followed men initially assessed in 1989/90, 1994/95 and followed up in 1998. OxLDL was found in 88 men with incident CHD and in 258 age- and survey-matched controls. OxLDL concentrations were significantly higher in subjects who subsequently experienced an event compared with controls. Plasma oxLDL was the strongest predictor of CHD events compared with a conventional lipoprotein-cholesterol profile and other traditional risk factors for CHD.10
At the 2004 American Heart Association Annual Scientific Sessions presenters
from Tufts – New England Medical Centre, reported on a meta-analysis of 17 major lipid
lowering trials involving 44,170 patients and involving 3,869 fatal or non-fatal heart attacks. They found that the increase in HDL was the best predictor of <b>decreased</b> risk of heart attack, and clearly a better predictor than lowering LDL. Their analysis also showed that there was no marked reduction in risk of heart attack until LDL was reduced by more than 30%.11 and 12
In the next article we’ll look more at different types of LDL, examine some new findings about a newly identified cysteine protein – resistin and its impact on triglycerides and LDL cholesterol. For the specific references to the medical journals used please email me at mcroger@shaw.ca . Yours in health and wellness, Roger.
© Roger Elmes 2016
——————————————————————————————
References
- Proc Jpn Acad Ser B Phys Biol Sci86(5); May 11, 2010
- Biol. Chem 1949: 179, 973–979
- Science 1950: 111, 166–171
- Science August 1947.
- Curr Opin Lipidology 2008;19:355-361 http://journals.lww.com/co-lipidology/Abstract/2008/08000/Association_of_fasting_and_nonfasting_serum.6.aspx
- Curr Opin Cardiol. 2009 July; 24(4): 345–350
- Mayo Clinic http://www.mayoclinic.com/health/vldl-cholesterol/AN01335 )
- N Engl J Med</i> 1997; 408-416
- <i>J Amer Coll Cardiol </i>1997; 30(2):392-9
- <i>Circulation</i>. 2005;112: 651-657
- (<I>Circulation</i> 2004; 110:11-813 Abstract 3754 and (10)
<i>Circulation(</i> 2004; 110: 227-239